When doctors told me there was nothing they could do to save my baby, I had to make an impossible choice: end our baby’s life, knowing I’d never be pregnant again or continue a pregnancy knowing that my baby would never survive.
Four years on I still can’t comprehend how I walked into the operating theatre pregnant and left with nothing but silence.
Losing a baby is devastating in any circumstance, but when that loss comes through termination for medical reasons, it becomes something else entirely; a complex, lonely kind of grief that doesn’t quite fit anywhere.
But, as Baby Loss Awareness Week comes to an end, we mustn’t exclude women like me.
Our loss, our pain, is as valid as anyone’s.
I first learned that getting pregnant would be a struggle for me when I was 27 when, after a decade of fighting for a diagnosis, I was told that I suffer with severe stage 4 endometriosis – the most advanced stage of the disease which is characterised by deeper growths in the structures of the pelvis and abdomen such as the bowel, bladder, and blood vessels.
As a result, my organs had been compromised by the disease and my fertility destroyed.
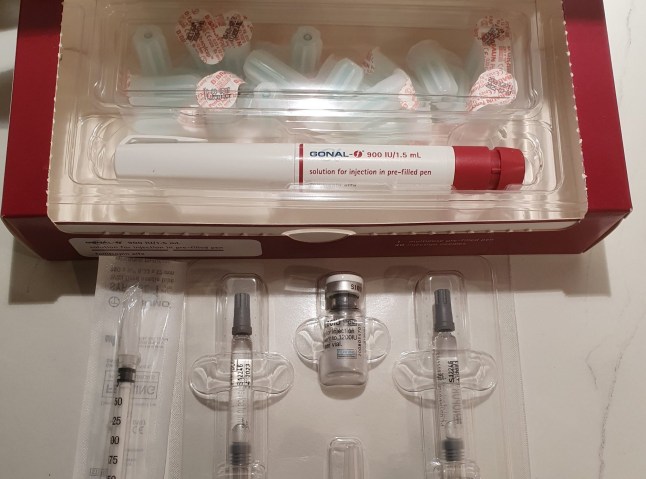
If I ever wanted to have a baby, IVF would be my only option. It was an overwhelming reality to comprehend, but I still had hope.
However, when my husband and I started our self-funded fertility journey in 2018, when I was 32, it was a struggle from the start.
For four years we endured round after round of hope, hormones, scans and tears. Each negative pregnancy test was another blow emotionally and financially.
Eventually though, on our sixth cycle, having spent approximately £54,000, we saw those two pink lines appear on a test. It was such a shock.
At first, the pregnancy was relatively easy as I didn’t suffer from morning sickness or fatigue, but I remained cautious, never allowing myself to think beyond each week.
That caution led me to get a private scan at 18 weeks – at which the sonographer flagged an issue with the baby’s bladder and advised me to get in touch with my midwife.
After begging the maternity team to give me my 20 week scan early, we learned the devastating news that our baby had Posterior Urethral Valves (PUV) – a rare condition where an obstruction in the urethra makes it difficult for urine to pass from the bladder causing kidney damage and preventing the lungs from developing.
The damage to our baby’s kidneys was so extensive that I was told they wouldn’t survive and that I’d have to make the decision no parent should ever face; to end our baby’s life.
For me, this decision was made harder by the fact I knew there would be no ‘next time’, no rainbow baby, no second chance. This was it.
Understanding Endometriosis
- Endometriosis is a chronic condition where tissue similar to the lining of the womb grows outside it.
- This tissue can be found on the ovaries, fallopian tubes, or even distant areas like the lungs.
- Endometriosis affects roughly 10% (190 million) of reproductive age women and girls globally
- It causes a variety of symptoms, including severe pain, heavy periods, and infertility.
- Find out more here
In having a termination for medical reasons (TFMR) I was effectively closing the door on my chance to ever carry my own child, for good.
The pain was overwhelming but I chose our child’s peace over my pain, and I have never regretted it.
Language immediately turned clinical – where everyone had been saying ‘baby’, now, suddenly, doctors referred to it as a ‘foetus’ and the warmth disappeared. It wasn’t meant to be cruel, but it stung.
I also wanted reassurance, someone to tell me it was the right thing to do. But it never came.
Doctors can only tell you the risks, odds, and facts of your baby’s diagnosis, they can’t decide for you. I understood why, but it didn’t make it any easier to have to find that comfort within myself.
Even after I’d made that painful ‘choice’ though, things were far from smooth.
Due to my complicated gynaecological history, I was advised to not give birth naturally. But when it came to TFMR, my hospital refused a surgical termination beyond 14 weeks – I was 21 weeks pregnant.
Baby Loss Awareness Week
- Baby Loss Awareness Week occurs annually from October 9th to October 15th.
- This week aims to raise awareness of pregnancy and infant loss and offer support to grieving families.
- The week concludes with the Wave of Light on October 15th, where candles are lit worldwide in remembrance.
- The week includes educational events and campaigns to reduce stigma and encourage open discussions about baby loss.
- Find out more here
Despite the baby loss charity, Tommy’s saying before 24 weeks you should be given the option, I was simply told they ‘did not perform that procedure’ and that only select hospitals would provide a surgical termination at that point.
I was then referred to an abortion clinic for a medical termination by my hospital – let’s be clear though, a TFMR is not a choice, it’s a medical necessity – but they couldn’t help either because of complications relating to my endometriosis.
My only remaining option was to induce labour even though that could lead to serious complications. It took two weeks to find a hospital that was willing to take my case on and perform the surgical termination.
At the hospital, the heartbreak only worsened.
Keep up with the conversations shaping Britain
Hi, I’m Ross McCafferty, Metro’s acting first-person and opinion editor.
Here at Metro, we’re passionate about giving a platform to unheard voices. You can read more real-life stories like this one with our News Updates newsletter.

We help people from all walks of life tell stories that inspire, educate and spark change. Sign up now to read them.
First, I had to explain out loud at reception, surrounded by women cradling newborns, why I was there. It was cruel and yet another reminder that TFMR sits in the shadows of both maternity and miscarriage care.
Then, after the surgery, my milk came in. I’d been told bleeding was expected, but no one had warned me about this painful and brutally ironic part. What’s worse, I later found out there’s medication to prevent it, but it was never offered to me.
And, while in the throes of grief and recovery, I also had to choose what happened next: burial, cremation, or sensitive disposal by the hospital. This conversation, unsurprisingly, remains a complete blur to me.
As alone as I felt at the time though, my experience is not unique: each year, it’s estimated 5,000 women across the UK face the devastating reality of having to end a wanted pregnancy due to a severe medical diagnosis.
I hope care and support has improved since my experience, but despite its prevalence I know that the silence hasn’t changed.
Too often, women facing TFMR feel isolated, judged or left to navigate the system alone, but our loss is as valid as any.
In fact, sometimes, resilience isn’t about holding on, it’s about knowing when to let go.
Do you have a story you’d like to share? Get in touch by emailing Ross.Mccafferty@metro.co.uk.
Share your views in the comments below.




Write Reviews
Leave a Comment
No Comments & Reviews