8 Oct, 2025 | Admin | No Comments
I’m a shopping editor and these are my picks for the final day of Amazon Prime


Metro journalists select and curate the products that feature on our site. If you make a purchase via links on this page we will earn commission – learn more
After covering Amazon Prime Day for over five years, I’ve learned a thing or two about how to shop it smartly.
I’ve also learned that Amazon sells way more than you might expect – from your favourite Redken shampoo to dishwasher tablets, method cleaning sprays to everyone’s favourite Italian spritz, and of course, the humble toilet roll.
Now that I’ve bought my first flat, I’m more conscious of what I’m spending. But with over a decade of shopping and writing under my belt, I’ve got a pretty good sense of what’s actually worth adding to your basket – and what’s just going to gather dust.
Shop these Amazon Prime Day deals while you can
- We’re spotlighting the best Prime Day deals from beauty to home tech – here are the best
- Amazon shoppers can snag 5-star rated Simba mattress at 27% off in huge Prime deal
- My favourite luxury hair tool is currently over £100 off in the Amazon Prime Day sale
- Best Ninja Amazon Prime Day 2025 on airfryers, blenders, ice cream makers and more
This list isn’t full of flashy gadgets or impulse buys. It’s the practical stuff: micellar water, snacks, cleaning products, essentials you’ll use every day. Not the most glamorous, sure, but stocking up during Prime Day can save you a surprising amount – and cut down those last-minute supermarket dashes.
So, if you’re looking to make the most of the sales without wasting money, here are the things I genuinely think are worth buying.
My top Amazon Prime Day picks:

Nespresso Vertuo Next Coffee Machine by De'Longhi
The Nespresso Vertuo Next by De'Longhi is a great Prime Day buy if you want barista-style coffee at home without the fuss. It’s compact, easy to use, and brews a range of coffee sizes – perfect for busy mornings or weekend treats. With a solid discount, it’s a smart investment that’ll save you money on takeaway coffees in the long run.

Coca-Cola Zero Sugar Cherry 8 x 330 ml
Coca-Cola Zero Sugar Cherry (8 x 330ml) is a fizzy, cherry-flavoured soft drink with zero sugar and calories, offering a refreshing twist on the classic taste. It’s vegan-friendly, made with natural flavours and sweeteners, and currently available for around £3.30.

Fairy Non Bio Pods Washing Liquid Laundry Capsules
Fairy Non Bio Pods are a Prime Day essential if you want gentle, effective laundry care at a great price. They’re dermatologically tested, kind on sensitive skin, and still tough on stains – which is why they’ve been a staple in my cupboard for years. Stocking up during the sale means fewer last-minute supermarket runs and better value for money per wash.

Aperol Aperitivo 70CL
Aperol Aperitivo is one of those bottles that instantly makes your drinks feel a bit more special – and Prime Day is the perfect time to grab it for less. Whether you're mixing up a classic spritz or experimenting with summer cocktails, it’s a great staple to have on hand. It also makes a lovely gift, so it’s worth picking up while it’s discounted.

method Concentrated Laundry Detergent in Tropical Coconut Scent
Method’s concentrated laundry detergent delivers powerful cleaning at just 20°C, tackling tough stains, reviving colours, and reducing fabric bobbles. A small dose provides long-lasting fragrance, and when paired with matching fabric softeners, creates a harmonised scent experience. Made with creativity and care, it’s designed to uplift your laundry routine and your mood.

Andrex Family Soft Toilet Paper 24 Rolls
The Andrex Family Soft Toilet Paper 24-roll pack is one of those unglamorous but genuinely useful Prime Day buys. It’s soft, strong, and ideal for stocking up – especially if you’ve just moved or want to avoid those annoying last-minute supermarket runs. With a decent discount, it’s a smart way to save on something you’ll definitely use.

REDKEN All Soft Shampoo and Conditioner Set for Dry Hair, With Argan Oil
The REDKEN All Soft Shampoo and Conditioner Set is a brilliant Prime Day buy if your hair’s feeling dry or in need of a little TLC. Infused with argan oil, it leaves hair noticeably softer, shinier, and easier to manage – and it’s a salon-quality duo that usually doesn’t come cheap. If you’ve been eyeing it up, now’s the time to grab it while it’s on offer.

Finish Ultimate Infinity Shine Dishwasher Tablet
The Finish Ultimate Infinity Shine Dishwasher Tablets are a Prime Day essential if you want sparkling dishes with minimal effort. They tackle tough stains, leave glassware streak-free, and come in recyclable packaging – so they’re effective and a bit more eco-conscious too.

Shark CryoGlow LED Face Mask
The Shark CryoGlow LED Face Mask is one of those luxe beauty gadgets that actually lives up to the hype – and Prime Day is the perfect time to invest. It combines LED light therapy with cooling technology to help calm, firm, and brighten skin in just a few minutes. If you’re into skincare and want a salon-style treatment at home, this is a smart splurge while it’s on offer.

COLOR WOW Dream Coat Supernatural Spray
The COLOR WOW Dream Coat Supernatural Spray is a Prime Day favourite for good reason – it delivers sleek, frizz-free hair that genuinely lasts. I’ve used it before big events and humid days, and the results are consistently impressive, like a professional blow-dry in a bottle. If you want smooth, glossy hair without the salon price tag, now’s the time.

Dyson Airwrap i.d.™ Multi-Styler and Dryer
The Dyson Airwrap i.d.™ Multi-Styler and Dryer is a standout Prime Day buy if you’re after salon-level styling at home. It dries and styles without extreme heat, which means less damage and smoother results – plus, the intelligent features make it even easier to customise your look. If you’ve been waiting for the right moment to invest, a Prime Day discount makes it a lot more tempting.

Maybelline New York Lash Sensational Sky High Mascara
The Maybelline New York Lash Sensational Sky High Mascara is a brilliant Prime Day beauty buy if you want serious length and lift without splurging. It gives lashes a full, fluttery look that lasts all day, and the flexible wand makes application super easy.

Garnier Vitamin C Daily UV Brightening Fluid Sheer Glow
The Garnier Vitamin C Daily UV Brightening Fluid Sheer Glow is a brilliant Prime Day pick if you want lightweight sun protection with added skincare benefits. It gives skin a subtle glow while helping to even tone over time, thanks to the vitamin C. If you’re after an affordable SPF that wears well under makeup and doesn’t feel greasy, this one’s a no-brainer.

Garnier Micellar Cleansing Water
Garnier’s Micellar Water gently cleanses skin, removing dirt, oil, and makeup in one step. Its vegan, fragrance-free formula is suitable for all skin types and enriched with Botanical Glycerin for hydration. The product is also dermatologically tested, sustainably packaged, and Leaping Bunny approved.

Apple AirPods Pro 2 Wireless Earbuds
The AirPods Pro 2 feature advanced hearing health tools, superior noise control, and improved sound quality, thanks to the H2 chip.
They offer a customisable fit, are resistant to dust, sweat, and water, and provide personalised spatial audio.
With up to 6 hours of listening time and a versatile charging case, they ensure a seamless and immersive audio experience.
BaByliss Titanium Brilliance Curls (32mm)
The BaByliss 2357U Titanium Brilliance Curls features a 32mm polished titanium barrel for smooth, lasting curls.
With six digital heat settings up to 210 degrees, and an extra-long barrel, it’s perfect for longer hair.
The Advanced Ceramics heating system ensures fast heat-up and consistent styling.

Nestlé Cocoa Chocolate Biscuit Bars, 1.36 kilograms (Pack of 1) KitKat, Blue Riband, Toffee Crisp
Introducing the KitKat and Friends Big Biscuit Box! This display-ready box contains 69 Biscuit Bars in five delicious flavours: KitKat® 2 Finger Original Milk Chocolate, KitKat® 2 Finger Orange Milk Chocolate, KitKat® 2 Finger Dark, Blue Riband® Milk Chocolate, and Toffee Crisp® Milk Chocolate Biscuit. Perfect for stocking up the office biscuit drawer or treating friends and family, this box is free from artificial colours, flavours, and preservatives. Now, you can bring this joy to any gathering with an assortment of biscuits that everyone will love.

L'OCCITANE Verbena Shower Gel 250ml
The L'OCCITANE Verbena Shower Gel (250ml) is a refreshing, citrus-scented body wash made with organic verbena extract from Provence. It gently cleanses and tones the skin, leaving it lightly fragranced with lemon and herbal notes – perfect for a revitalising daily shower.

Always Sensitive Ultra Night Sanitary Towels with Wings, Size 3, 100 Towels (10 x 10 Packs)
Part of the Prime sale, the Always Sensitive Ultra Night Sanitary Towels with Wings (Size 3, 100 count) offer gentle overnight protection with a super absorbent core and soft comfort zones designed for sensitive skin. Each towel is ultra-thin, dermatologically tested, and individually wrapped for hygiene on the go – ideal for heavy flow nights at just £10 for 10 packs.
Follow Metro across our social channels, on Facebook, Twitter and Instagram
Share your views in the comments below
8 Oct, 2025 | Admin | No Comments
Where Dolly Parton is living amid health problems as sister asks for 'prayers'

Jolene singer Dolly Parton has postponed her Las Vegas residency amid health troubles – see the epic house in Nashville where she’s resting time
Queen Maxima of the Netherlands shimmered in a sequined electric pink fit-and-flare dress from Oscar de la Renta at the opening for the 20th edition of the Tilburg Trade Fair on Tuesday.
8 Oct, 2025 | Admin | No Comments
'My ex had the UK's biggest penis and it's ruining my new relationship'

A woman has revealed that when her new boyfriend discovered her ex was famous for having the biggest manhood ever, he started to act ‘weirdly’ and now she’s worried about their relationship
8 Oct, 2025 | Admin | No Comments
We’re spotlighting the best Prime Day deals from beauty to home tech – here are the best


Metro journalists select and curate the products that feature on our site. If you make a purchase via links on this page we will earn commission – learn more
Amazon has finally launched its hotly anticipated Prime Day sale. While the deals are flooding in thick and fast, products are equally whizzing off the shelves too.
With hundreds and thousands (maybe even hundreds of thousands) of products reduced across all categories, including beauty, fashion, home and technology, it can be overwhelming sifting through to find the best buys for you. But, we’re here to help.
We have sifted through all the deals on Amazon to find the absolute best bargains, the price drops on bestselling items, and flash deals to spotlight the best of the best. Take it as your one stop shop for everything Amazon to make your shopping spree a breeze.
From cleansers to TVs, take a look at the ultimate deals at Amazon this Prime Day and from big names too. Keep an eye out for GHD, CeraVe, as well as Apple, HiSense and much more.
Just in case you needed reminding, the sale runs from October 7 and 8, but stock is selling fast, and some deals may not last for the entire duration. Our advice: if you see a steal, don’t think twice.
Shop The Best Prime Day Deals
Beauty

St.Tropez Self Tan Express Mousse
If you want to faux the sunkissed look without laying out inharmful UV rays then a fake tan is a worthy investment. This Self Tan Express Mousse develops in one hour (though you can leave on for longer), and leaves a natural bronzed look. Plus it has been reduced by 63%.
Home

Echo Pop (Newest Gen)
If you are transforming your house into a smart home then it is worth investing in all the smart devices in the Amazon sale. The Echo Pop is a smart speaker, which is ideal for those who want extra surround sound when it’s movie night, or like to dance around to their favourite tracks. What we love is it is more discreet and takes up less space than a conventional speaker.
Technology

Apple AirPods Pro 2 Wireless Earbuds
Whether you are a music lover, enjoy a podcast or watching your favourite series on the go without disturbing others around you on the commute, Apple’s AirPods are the way to go. The design is lightweight and comfortable in your ear. Plus you are not restricted like wired headphones.
Do you have your eye on anything this Prime Day sale? Or are you waiting until the end of the week? Let us know everything in the comments below!
Follow Metro across our social channels, on Facebook, Twitter and Instagram
Share your views in the comments below
8 Oct, 2025 | Admin | No Comments
Amazon just dropped the price of Ring doorbells in its huge October sale – now 39% off

Metro journalists select and curate the products that feature on our site. If you make a purchase via links on this page we will earn commission – learn more
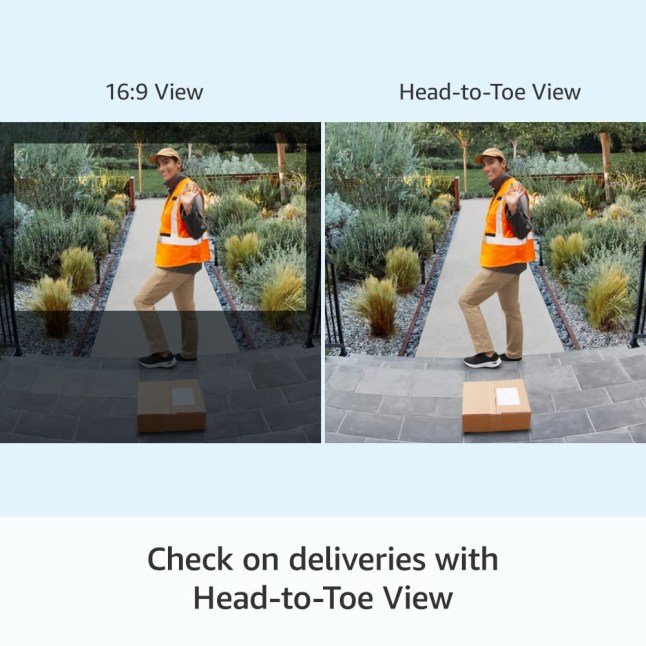
Those looking to up their home security will be pleased to hear that the Ring Battery Video Doorbell Plus by Amazon is available at its lowest price ever – for just £79 (down from £129.99), during October’s Amazon Prime Big Deal Days.
Not to mention even cheaper than last year’s sale – and it was at a record low then.
To make things even better, you don’t even need to be a Prime member to make the most of this limited-time offer – how good!
Now with £50.99 off, the popular wireless video doorbell camera with 1536p HD video helps you see who’s at your door more clearly than ever.

Ring Battery Video Doorbell Plus by Amazon
The latest battery-powered Ring doorbell features 1536p HD+ video for a clear view of visitors and deliveries. It has an improved battery life, motion detection with custom zones, two-way talk, and Quick Replies for when you can’t answer. Includes enhanced night vision, real-time notifications, and easy, wire-free installation. Plus, it’s compatible with Alexa for voice alerts and live view.
With an average score of 4.5/5 stars, over 3,190 people have been quick to leave their thoughts on the nifty doorbell device with a whopping 72% of people giving it the full five-stars.
One person just named ‘Amazon Customer’ said: ‘The ring doorbell is great; you can see everything from top to bottom. Easy set up. The sound is great. I got the ring doorbell at a good price. So very please. Performance is good.’
Linda Neilson followed suit and added: ‘This is an absolutely brilliant system and one of the best things we’ve bought this year. It gives us an update on who’s at the front door and if by any chance we’re not home we can tell them to leave a message or to put things in the delivery box at the front door.’
‘The Ring battery-operated doorbell has exceeded my expectations. The battery life is impressive, even with settings that typically consume more power,’ added Claudisabel.
Elaine Gleeson also mentioned: ‘The Ring Doorbell is fantastic, and the chime is essential. It definitely gives peace of mind, and you know when someone is approaching your door which is fantastic. I would definitely recommend it!’
What makes the device so handy whether you’re at home or away is the fact you can keep an eye on packages at your doorstep with the enhanced Head-To-Toe View, providing an expanded outlook. It’s never been easier to stay informed with real-time alerts sent directly to your smartphone whenever someone presses your Video Doorbell or motion is detected.
As for when night falls, the Colour Night Vision feature ensures you never miss a moment, even in the dark. If your hands are full, you can answer the door using the Quick Replies feature, available with a Ring Protect subscription.
Better yet, installation is simple thanks to the Quick Release Battery Pack. All you need to do is pair your device with a Ring Chime or a compatible Alexa-enabled device to receive audio notifications throughout your home.
It’s that easy.
Oh, and standard features such as real-time notifications, Live View, and Two-Way Talk are included at no additional cost on all compatible Ring devices.
Get ready to enhance your experience with a Ring Protect Plan (subscription sold separately) to record, review, and share the moments you missed. A 30-day free trial is included with your purchase.
Sold.
Follow Metro across our social channels, on Facebook, Twitter and Instagram
Share your views in the comments below
8 Oct, 2025 | Admin | No Comments
Amazon shoppers can snag 5-star rated Simba mattress at 27% off in huge Prime deal

Metro journalists select and curate the products that feature on our site. If you make a purchase via links on this page we will earn commission – learn more
Permanently exhausted and not sleeping well? The culprit could be your old, lumpy mattress.
Make no mistake about it, a good night’s sleep is important. That’s why, savvy shoppers, you’ll be pleased to hear about big savings happening at Amazon for its October Prime Big Deal Days, especially on the cult-status Simba Hybrid Pro mattress.
Normally priced at a premium, during this Prime Big Deal Days event you can snap up a Simba Hybrid Pro mattress for a fraction of the price.
The Simba Hybrid Pro mattress is designed to provide an exceptional sleeping experience with its innovative features. At the top, a breathable, pure wool layer ensures a fresher sleep by naturally regulating temperature and wicking away moisture. This helps keep you comfortable throughout the night, regardless of the season.
Top rated with hundreds of 5* reviews, this mattress should come with a warning – you’ll never want to get out of bed.
Beneath the wool layer, the mattress boasts a double layer of 2,000 zoned, titanium alloy Aerocoil springs. These springs are strategically placed to adapt to your body’s contours, offering superior spinal alignment and pressure relief. This extra spring layer ensures that your body is well-supported, reducing the chances of waking up with aches and pains.
For those who tend to sleep hot, the open-cell Simbatex foam is a game-changer. This foam promotes optimal airflow and efficiently dissipates heat, helping you stay cool and comfortable all night long.
The mattress also features 100% edge-to-edge support, thanks to the SupportCore base. This base prevents roll-off at the sides and enhances the overall durability of the mattress, ensuring consistent support across the entire surface.
Additionally, the Simba Hybrid Pro comes with a soft, knitted top cover that is both comfortable and practical. The cover zips off easily, making it simple to wash or replace, so your mattress stays fresh and clean.
Better yet? Proudly made in the UK, the Simba Hybrid Pro mattress supports local manufacturing and helps reduce transport emissions, contributing to a more sustainable future.
This mattress is not only designed for comfort but also with a commitment to environmental responsibility.
Plus there are also plenty of sizing options are available to suit your bed frame and it’s incredibly comfortable whether you’re a side, back or front sleeper.
We’re not the only ones raving about the mattress as one reviewer said their ‘Back pain had disappeared!’ With another saying ‘It’s a dream to sleep on.’
A third reviewer even claimed ‘At last I found the mattress I have been after for a long time! I can’t believe my luck! I slept like a baby and the next morning I felt well and incredibly less back/neck pain than usual!’
Intrigued? Don’t sleep on this deal. Head to Amazon sharpish and snap up a Simba Hybrid Pro mattress before time runs out – at 11:59pm this October 8.
Follow Metro across our social channels, on Facebook, Twitter and Instagram
Share your views in the comments below
8 Oct, 2025 | Admin | No Comments
EXCLUSIVE: Flowerbx's Whitney Hawkings opens the doors to her stunning six-storey Chelsea home

HELLO! takes a look inside the London home Flowerbx founder Whitney Hawkings shares with her fashion designer husband, former Tom Ford creative director Peter Hawkings.
7 Oct, 2025 | Admin | No Comments
Meghan Markle's fans leap to her defence over 'endearing' kitchen faux pas

The Duchess of Sussex has sparked a debate on social media after she was pictured using a special tool to make her preserve – some say she was doing it all wrong
7 Oct, 2025 | Admin | No Comments
Earl Charles Spencer reveals 'privileged' link to late Jilly Cooper in subtle tribute

Princess Diana’s brother, Earl Charles Spencer, has revealed a previously unknown link to the late Jilly Cooper after the author’s death aged 88.