21 Jan, 2026 | Admin | No Comments
Inside Nicola Peltz’s tactical mirroring of mother-in-law Victoria Beckham

Brooklyn Beckham’s wife, Nicola Peltz, had a great relationship with her mother-in-law, Victoria Beckham, and has often worn the same outfits as the former Spice Girl.
The King’s residence, Buckingham Palace, had a surprising visitor running around the grounds, inside the gates– and members of the public were left shocked
21 Jan, 2026 | Admin | No Comments
Baggy jeans are ‘out’ – here’s the iconic French fashion style replacing them

Baggy, wide-leg jeans are no longer as fashionable as they once were. The stylish cut of the ‘cigarette pant’ is far trendier for 2026, and it’s a French fashion staple.
21 Jan, 2026 | Admin | No Comments
Geena Davis’ $5.6m Mediterranean mansion in coveted California neighbourhood sold in just two months – details
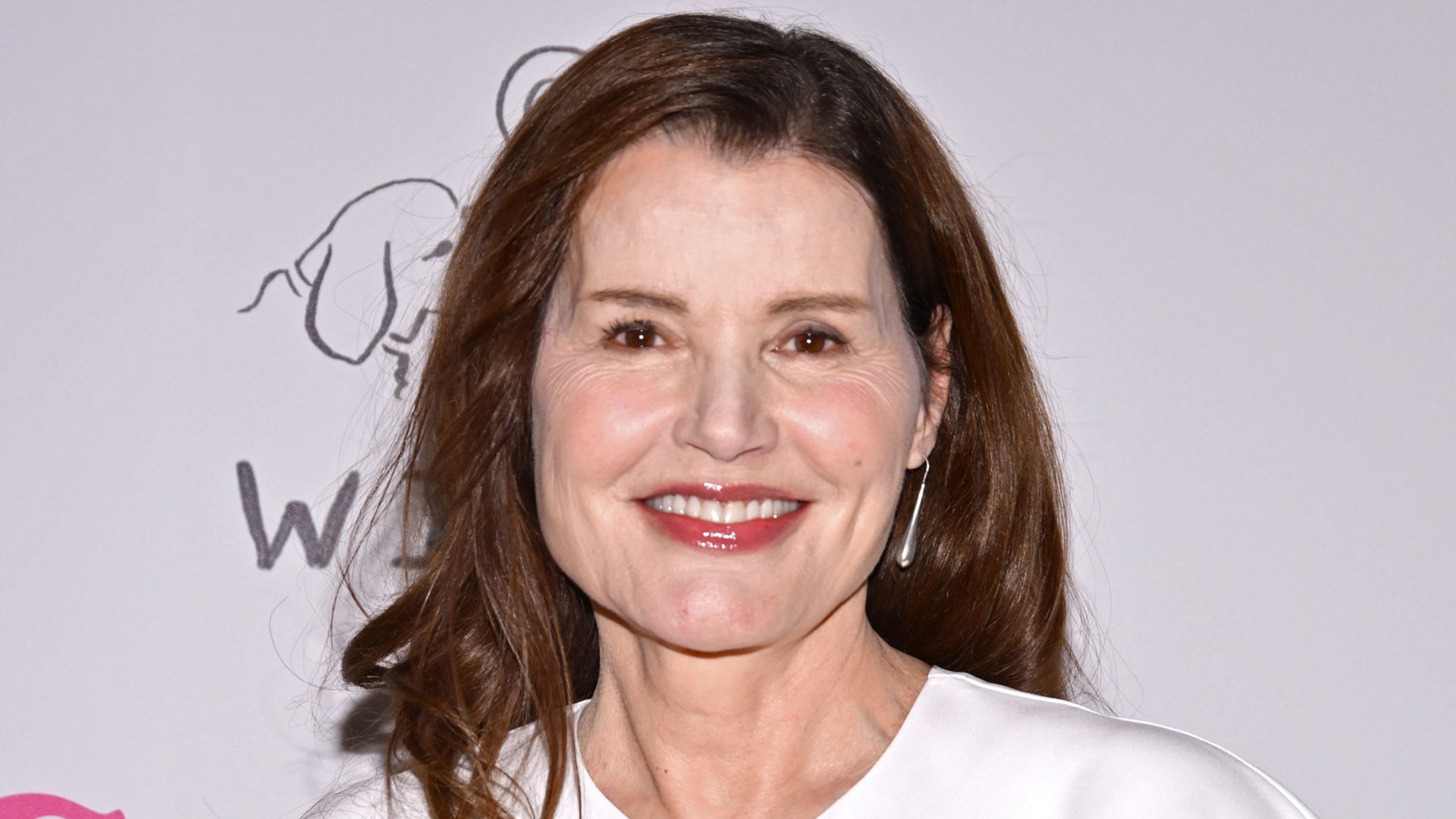
Thelma & Louise star Geena Davis, who turns 70 today, owned a $5.6m Mediterranean mansion in coveted California neighbourhood – that sold after two months on the market.
21 Jan, 2026 | Admin | No Comments
Princess Kate wears Zara for the first time in a year – and it only cost her £26

The Princess of Wales looked stunning in a tartan coat on a visit to Scotland, and underneath her statement look was a Zara rollneck that you can pick up for £25.99
King Charles is giving his brother Andrew a safe haven at Sandringham, but he’s forbidden him from having this one thing
21 Jan, 2026 | Admin | No Comments
Leggy Christie Brinkley does DIY in a bikini at Turks & Caicos home

Christie Brinkley put on a very leggy display as she did DIY in a bikini inside her stunning Turks & Caicos home
21 Jan, 2026 | Admin | No Comments
Why Huawei’s FreeClip 2 are the perfect everyday headphones for 2026

Metro journalists select and curate the products that feature on our site. If you make a purchase via links on this page we will earn commission – learn more
Finding the right pair of headphones can feel surprisingly overwhelming. With so many options on the market – many of them promising similar features – it’s hard to know which ones are actually worth your time.
That said, there are a few brands that consistently stand out for getting the balance right between innovation, design, and performance, and HUAWEI is firmly one of them.
Enter the HUAWEI FreeClip 2. Following the success of the original FreeClip launch in 2023, this updated version builds on what worked well the first time around, with thoughtful refinements that show HUAWEI’s growing confidence in the open-ear space. The result is a pair of headphones that feel considered, comfortable, and refreshingly different.
These aren’t your typical in-ear buds. The FreeClip 2 is an open-ear wireless design that puts just as much emphasis on style as it does on sound. The updated Airy-C bridge has been reworked to feel lighter and more discreet, making them easy to wear all day – whether you’re commuting, working, or heading out for a walk. They sit more like a sleek accessory than a piece of tech, which will appeal to anyone who wants their headphones to blend seamlessly into their look.
Best of Metro Deals
Get exclusive discounts with Metro Deals – save on getaways and spa days. Powered by Wowcher
Bannatyne Spa
Spa day for two with treatments, lunch & prosecco — save up to 57% off.

Other deals
Mystery Escape
Hotel stay with return flights from as low as £92pp — save on worldwide holiday packages.
Beach Retreat (Lanzarote)
4* Lanzarote beach holiday with flights — save up to 58%.
UK Getaway
4* Radisson Blu Durham stay with breakfast, spa access & late checkout — save 60% off.
Drive Supercars
3–12 lap supercar driving experiences from £16.99 — save up to 65%.
Sound-wise, the FreeClip 2 doesn’t disappoint. The dual-diaphragm driver helps create a more immersive listening experience, while the compact acoustic ball inside the earbud works to deliver clear, balanced audio. Despite their small size, there’s an impressive level of depth and clarity, making them well-suited to everything from music and podcasts to audiobooks and calls.
Compared to the first generation, comfort has clearly been a priority this time around. The new design offers improved flexibility and is around 25% softer, thanks to the use of liquid silicone and shape-memory materials. HUAWEI also tested the fit on over 10,000 ear samples worldwide, which shows how securely they’ll sit. Whether you’re running, cycling, dancing, or simply navigating a busy commute, they stay comfortably in place without feeling intrusive or falling out.
The FreeClip 2 comes in blue, white, and black, retailing for £179.99, with a rose gold option set to follow soon. Battery life is another strong point, offering up to nine hours of continuous playback, extending to 38 hours when used with the charging case. A quick 10-minute charge also provides around three hours of listening time, ideal for those moments when you’re rushing out the door.
Available exclusively via the Huawei Store, early buyers can take advantage of a £20 launch coupon until March 1, alongside 12 months of Loss Care and 10x HUAWEI Reward Points to put towards a future purchase.
Better yet? There’s also a limited‑edition bundle on offer, which includes two pairs of FreeClip 2 earphones plus a chic set of Les Néréides earbud accessories (worth up to £80) for £319 — a saving of up to £120.
Surely you’re tempted now, right?
Overall, the HUAWEI FreeClip 2 feels like a brilliant evolution rather than a complete reinvention. It’s a smart option for anyone curious about open-ear headphones, or for those who want something comfortable, stylish, and easy to wear throughout the day – without compromising on sound quality.
Follow Metro across our social channels, on Facebook, Twitter and Instagram
Share your views in the comments below
His Majesty King Charles III’s Gloucestershire estate has a packed calendar of events, including an end of winter workshop
21 Jan, 2026 | Admin | No Comments
Woman’s ‘genius’ Hinge prompt has men literally lining up outside her door

A woman was fed up of wasting her time meeting men who she didn’t have a spark with, so decided to take matters into her own hands with a ‘genius’ prompt on Hinge





